The healthcare industry might look like it’s blooming, and advancements are on the rise since COVID-19 but conglomerates and small businesses are still yet to reach their full potential and scale at large.
Why?
APIs are fast and perfect for building scalable applications and helps fasten the communication process between two systems. Most people think APIs are just about building and deploying, but it’s way more than that.
API testing is one of the most crucial aspects of using APIs, you need to set the rules, test the limits and ensure that your APIs are safe, scalable and efficient.
Even better the numbers back it up. The API testing market is set to show an exponential growth from $1.07B to $4.73B (2022-2030).
While the figures are promising, 64% of users still don’t check their APIs as thoroughly as they should.
API testing isn’t just another trending topic. It’s your business’s credibility in line, so plan to build systems that helps save time and get more customers.
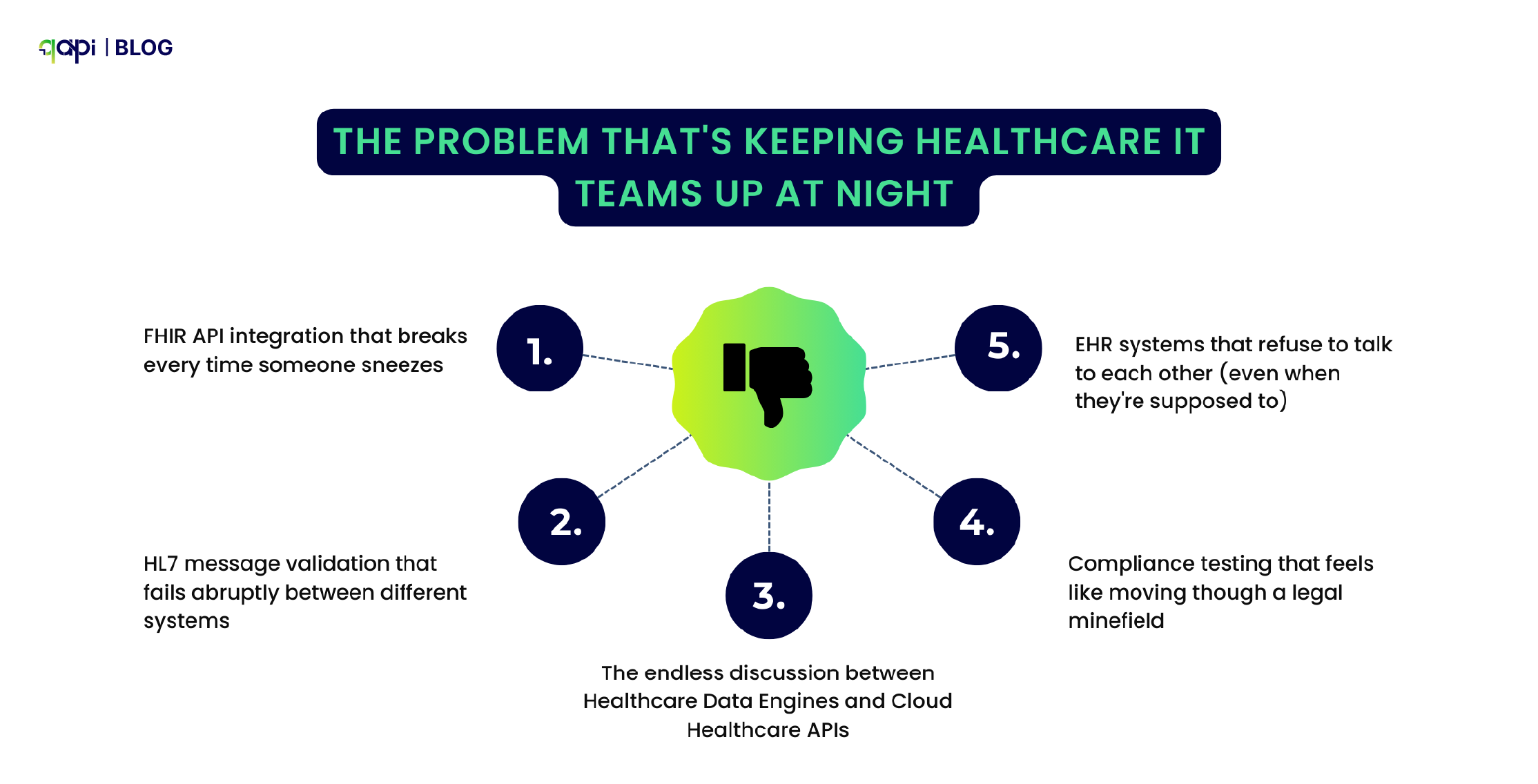
The Problem That’s Keeping Healthcare IT Teams Up at Night
Let’s be honest – healthcare APIs are a nightmare to test. While everyone’s talking about digital transformation and connected care, the reality on the ground is far messier.
Just scroll through Stack Overflow or Reddit, and you’ll find developers pulling their hair out over:
• FHIR API integration that breaks every time someone sneezes
• HL7 message validation that fails abruptly between different systems
• The endless discussion between Healthcare Data Engines and Cloud Healthcare APIs
• Compliance testing that feels like moving though a legal minefield
• EHR systems that refuse to talk to each other (even when they’re supposed to)
And here’s the ice breaker – research shows that 37% of organizations consider security as their top API challenge, and API breaches leak 10 times more data than your average security incident.
In healthcare, that’s not just embarrassing – it’s potentially life-threatening.
When APIs Fail, People Get Hurt
As simple as that.
Let me tell you about a major hospital network. They were drowning in API integration problems, and it wasn’t just a technical headache – it was a patient safety crisis waiting to happen.
Their daily routine looked like this:
• 15% of patient records were showing incomplete data (imagine trying to treat someone when you can’t see their full medical history)
• Critical lab results were delayed by 3 hours on average (in emergency medicine, that’s an eternity)
• Staff were spending 40 hours per week manually fixing data that should have flowed seamlessly between systems
• They were having near-miss medication errors because APIs were passing along inconsistent patient allergy information
Then came the breaking point.
During what should have been a routine system upgrade, their API endpoints started returning inconsistent FHIR resource formats. Their QA team was doing their best with manual testing, but let’s face it – manually testing every possible combination of patient data scenarios is impossible.
They missed edge cases in patient allergy data transmission. There was one patient with a severe penicillin allergy almost received exactly that medication because the API “forgot” to pass along that critical information between systems.
That’s when they realized manual testing wasn’t just inefficient – it was dangerous.
Here’s how it went down
The Patient Allergy API: What Should Have Happened vs. What Actually Happened
What Actually Should Have Happened
Step 1: Doctor prescribes penicillin
• Prescription system calls: GET /api/patient/12345/allergies
Step 2: Allergy API responds correctly
{ “patient_id”: “12345”,
“allergies”: [
{
“allergen”: “penicillin”,
“severity”: “severe”,
“reaction”: “anaphylaxis”
}
]
}
Step 3: Prescription system processes response
• Checks prescribed medication against allergy list
• Finds penicillin match
• Triggers alert: “SEVERE ALLERGY WARNING”
• Blocks prescription until doctor acknowledges
Step 4: Doctor gets immediate warning
• Prescription system shows red alert
• Doctor selects alternative drug/medicine
• Patient receives safe medication
What Actually Happened
Step 1: Doctor prescribes penicillin
• Prescription system calls: GET /api/patient/12345/allergies
Step 2: Allergy API returns faulty response
{ “patient_id”: “12345”,
“allergies”: null
}
Instead of the expected allergy data
Step 3: Prescription system misinterprets response
• Receives “allergies”: null
• Here the system references “no allergies” instead of “data unavailable”
• No allergy check performed
• No alerts were triggered
Step 4: Dangerous prescription proceeds
• System shows “No known allergies”
• Doctor proceeds with penicillin prescription
• Patient nearly receives potentially fatal medication
Why Focusing on API Testing Made a difference
Here’s where things get interesting. Instead of throwing more people at the problem or buying another expensive tool that would gather dust, they decided to try something different: AI-powered API testing.
Smart Test Generation That Actually Makes Sense AI analyzed their FHIR schemas and automatically generated comprehensive test cases covering every resource type and edge case they could think of (and plenty they couldn’t). No more manually writing test scripts for the 100th time.
Predicting Problems Before They Become One qAPIs learning models, once trained on historic healthcare data patterns, started predicting potential integration failures. It’s like having a streetlight on an empty road – the system could spot trouble brewing before patients were affected.
Compliance Testing Made Things Easier AI-driven validation started ensuring HIPAA, FDA, and interoperability standards compliance automatically. What used to take two weeks now takes two hours.
24/7 Monitoring Continuous monitoring began identifying unusual API behavior patterns that could indicate data corruption. The staff was able to run tests round the clock to match the backlog and also analyse the tests with increased visibility.
The Results That Actually Matter
Six months later, here’s what changed:
• 95% reduction in data integration errors (that’s not a typo)
• Real-time detection prevented multiple potential patient safety incidents.
• Compliance testing went from 2 weeks to 2 hours (giving QA teams their lives back)
• API reliability improved to 99.9% uptime (because when you’re dealing with health data, “good enough” isn’t good enough)
What This Means for Your Healthcare Organization
Look, every healthcare organization is dealing with some version of this problem. Whether you’re a small clinic trying to get your patient portal to talk to your EHR, or a major health system juggling dozens of different APIs, the challenges are real.
The old approach of manual testing and hoping for the best isn’t just inefficient anymore – it’s becoming ethically questionable. When lives are on the line, can we really afford to test APIs the same way we did five years ago?
The bottom line: AI-powered API testing isn’t just about making developers’ lives easier (though it does that too). In healthcare, it’s about making sure that when a doctor needs critical patient information, the APIs deliver it accurately, completely, and on time.
Because at the end of the day, behind every API call is a human being who needs care. And they deserve better than crossed fingers and manual testing.
qAPI is an end-to-end API testing tool that acts as a one stop solution for all your API testing needs. No more switching between tools, just simple, streamlined tests in minutes.
What’s your biggest healthcare API testing challenge? Let’s talk reach out to us at marketingqapi@qyrus.com